Stem cell model offers clues to cause of inherited ALS
23 Jun 2011
An international team of scientists led by researchers at the University of California, San Diego School of Medicine have used induced pluripotent stem cells (iPSCs) derived from patients with amyotrophic lateral sclerosis (ALS) to reveal for the first time how reduced levels of a specific protein may play a central role in causing at least one inherited form of the disease.
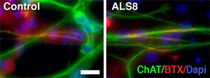 |
| Motor neurons (green) derived from ALS induced pluripotent stem cells forming neuromuscular junctions (red). Image courtesy of Alysson Muotri, UCSD. |
The work, published in the June 2011 online issue of the journal Human Molecular Genetics, could help scientists overcome a major hurdle in the study and treatment of ALS, an incurable neuromuscular disorder also known as Lou Gehrig's disease. ALS is universally fatal, with a median age of onset of 55 years and survival of two to five years after symptoms appear. Past research efforts have long been stymied by difficulties in translating successful drug tests in animal models of ALS to humans.
''There is an urgent need for ALS human models that can be translated into clinical trials to verify therapeutic targets in the human genetic background,'' said Alysson R. Muotri, PhD, assistant professor in the UCSD Departments of Pediatrics and Cellular and Molecular Medicine, and one of the study's senior authors. ''Rodents have been used in the past and still have a critical impact in unveiling the complexity of ALS, but the vast majority of drugs that have demonstrated efficacy in rodent models have not done the same in preclinical and clinical human trials.''
In the new work, Muotri and colleagues turned to iPSCs derived from the skin cells of patients with a familial form of ALS called ALS8 to create motor neurons that provided a novel in vitro model of the disease. iPSCs from ALS patients have been described before, but finding cellular and molecular phenotypes has proved to be a continuing challenge. The use of a familial form of ALS offered an advantage since the mutated gene could be tracked during motor neuron differentiation.
''We don't know what causes most cases of ALS, but for roughly 10 percent of patients with ALS, the disease is the result of inherited genetic mutations,'' Muotri said. ''One of these familial forms is ALS8, which results from mutations in the VAPB gene. Using iPSCs from several patients from two independent families, we found that VAPB protein levels are reduced in ALS8-derived motor neurons compared to similar cells from non-carrier siblings of ALS8 patients.''
Muotri said the finding suggests reduced VAPB protein levels may be a key to the development of ALS8 and perhaps other forms of the disease as well, including sporadic or non-hereditary ALS, where reduced VAPB protein levels have also been documented.


















