Immune mechanism blocks inflammation generated by oxidative stress
By By Scott LaFee | 07 Oct 2011
Conditions like atherosclerosis and age-related macular degeneration (AMD) – the most common cause of blindness among the elderly in western societies – are strongly linked to increased oxidative stress, the process in which proteins, lipids and DNA damaged by oxygen free radicals and related cellular waste accumulate, prompting an inflammatory response from the body's innate immune system that results in chronic disease.
In the 6 October 2011 issue of Nature, researchers at the University of California, San Diego School of Medicine, as part of an international collaborative effort, identify a key protein that binds to a molecule generated by oxidative stress, blocking any subsequent inflammatory immune response.
The scientists, led by senior author Christoph J. Binder, assistant adjunct professor of medicine at UC San Diego, principal investigator at the Centre for Molecular Medicine of the Austrian Academy of Sciences and professor at the Medical University of Vienna, say their findings reveal important insights into how the innate immune system responds to oxidative stress and might be exploited to prevent and treat AMD and other chronic inflammatory diseases.
Degeneration
Age-related macular degeneration (AMD) gradually destroys sharp, central vision. It is the most common cause of blindness among the elderly. There are two forms: dry AMD and the typically more severe and faster-acting wet AMD. In dry AMD, light-sensitive cells in the center of the retina slowly break down, obscuring central vision. In wet AMD, abnormal blood vessels grow under the retina, leak and disrupt vision. In this image, drusen – yellowish deposits of cellular debris – accumulate in a case of dry AMD.
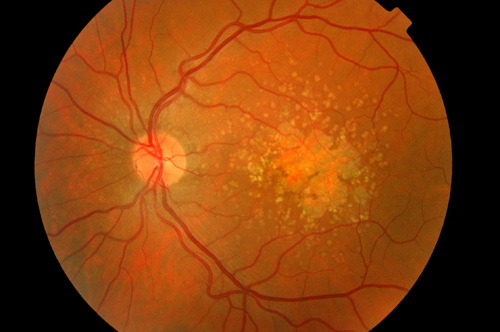 |
| Age-related macular degeneration (AMD) gradually destroys sharp, central vision. It is the most common cause of blindness among the elderly. There are two forms: dry AMD and the typically more severe and faster-acting wet AMD. In dry AMD, light-sensitive cells in the center of the retina slowly break down, obscuring central vision. In wet AMD, abnormal blood vessels grow under the retina, leak and disrupt vision. In this image, drusen – yellowish deposits of cellular debris – accumulate in a case of dry AMD. |
Specifically, Binder, Joseph L. Witztum, professor of medicine at UC San Diego, and colleagues in Austria, Germany, England and Maryland discovered that when lipids (fats) in cell membranes degrade through oxidative stress, they produce a number of reactive products, including a compound called malondialdehyde (MDA), which in turn modifies other molecules to create novel oxidation-specific epitopes, the part of antigens that draws the attention and inflammatory response of the innate immune system.
The researchers noted, in particular, that MDA attracted an immune system protein called complement factor H (CFH), which bound to it, effectively blocking the uptake of MDA-modified proteins by macrophages, a type of white blood cell charged with killing and eliminating foreign invaders and substances. In in-vivo experiments, the researchers reported that CFH neutralised the inflammatory effects of MDA in mice retinas, limiting the inflammatory response associated with AMD and other chronic diseases.
They also found that a specific mutation in the CFH protein, which is associated with a four-to-seven-fold greater risk of developing AMD, greatly diminished the ability of CFH to bind to MDA.
Binder said the findings further demonstrate the innate immune system's important but not fully appreciated ''house-keeping function, defending against endogenous waste products and not just against foreign microbial products.''
Beyond that, he said the distinctive, protective role of CFH represents a potential new therapeutic approach for treating AMD, heart disease and other chronic conditions. ''This activity of CFH can be used for the development of neutralizing agents to mimic this function.''
Funding for this study came, in part, from the Austrian Academy of Sciences, the Austrian Research Promotion Agency, the Austrian Science Fund, the National Institutes of Health, the Edward N. & Della L. Thorne Memorial Foundation Awards Program in AMD Research, the Wilmer Eye Institute, the Deutsche Forschugsgemeinschaft, the ProRetina Foundation, the Fondation Leducq, the Wynn-Gund Translational Research Acceleration Program, the National Neurovision Research Institute, the American Health Assistance Foundation and the European Commission.
Co-authors of the paper are David Weismann of the Austrian Academy of Sciences and the Medical University of Vienna; Karsten Hartvigsen, Austrian Academy of Sciences, Medical University of Vienna and UC San Diego; Nadine Lauer, Christine Skerka and Peter F. Zipfel, Freidrich Schiller University, Jena, Germany; Keiryn L. Bennett and Giulio Superti-Furga, Austrian Academy of Sciences; Hendrik P.N. Scholl, Marisol Cano and James T. Handa, Johns Hopkins University; Peter Charbel Issa, University of Oxford, United Kingdom; Hubert Brandstatter, Medical University of Vienna; and Sotirios Tsimikas, UC San Diego.


















